General medicine case:
A 48 yrs old female with abdominal distension,and decrease in urine out put.
6/6/23
Hi iam Likitha 3rd semester student. This is an online elog book to discuss our patients health data after taking his consent, this also reflect my patient centered online learning portfolio.
Case sheet:
A 48 yrs old female, resident of panagallu came to medicine OPD with
Chief complaints of:
•Abdominal distension since 6 days
•SOB since 5days
•B/L lower limbs swelling
•Decrease in urine output since 3days
History of present illness:
Patient was apparently asymptomatic 6 days back, then she developed abdominal distension followed by SOB, pedal oedema and oliguria. Pedal oedema is bilateral , which is incidious in onset and pitting type.
History of past illness:
•K/C/O:DM( since 10 yrs)
NK/C/O:HTN/TB/Asthma/CAD/epilepsy
•she showed similar symptoms of abdominal distension, SOB, pedal oedema &decreased urine output 2 yrs back. She was diagnosed as CKD.
Personal History:
Married
Appetite:lost
Diet:mixed diet
Bowel movement:normal
Micturirion:normal
Sleep:normal
No addictions
No allergies
Family History:no significant family history
Drug History:
On metformin since, 10 yrs for DM.
Physical Examination:
General Examination:
Patient was conscious, coherent and cooperative
Pedal oedema : present
Pallor:present
No icterus
No cyanosis
No clubbing of fingers
No lymphadenopathy
Vitals:
Temperature: febrile
Pulse rate:89
RR:18 per minute
BP:130/70
Systemic Examination:
Cardiovascular system:
•cardiac sounds S1&S2 heard.
Respiratory system:
Central trachea
Dyspnea:present
Abdomen:
Distended abdomen
Tenderness:present
No palpable mass
No palpable liver and spleen
Bowel sounds heard
CNS:
Patient was conscious conscious
Normal speech
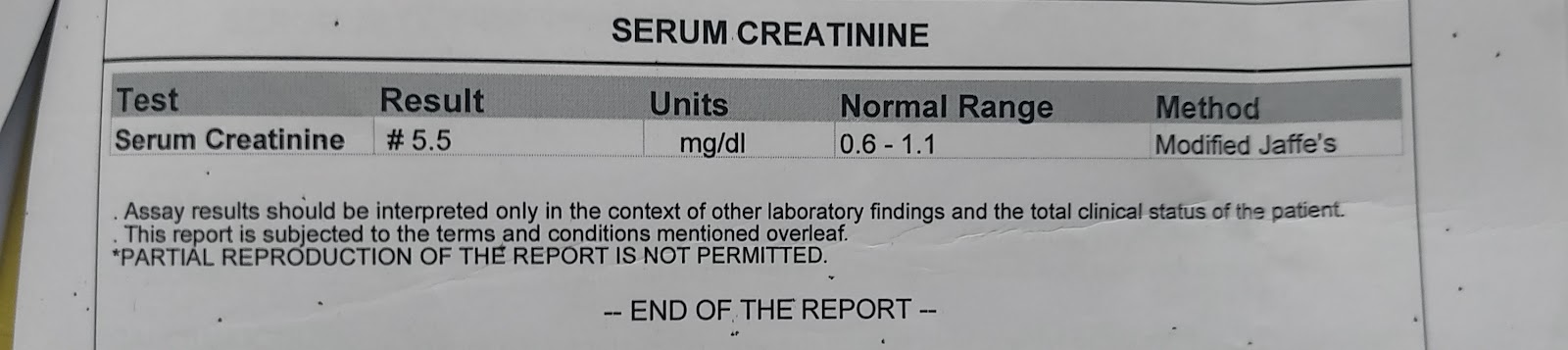
Investigations: